The Promise of Brain Implants in Addiction Therapy
Addiction is a complex and debilitating disorder that affects millions of people worldwide, often leading to devastating consequences for individuals and their communities. Traditional treatment approaches, such as counseling and medication, have shown limited success in managing addiction, highlighting the urgent need for innovative interventions. In recent years, researchers have turned to cutting-edge technologies, such as brain implants, as potential tools for treating addiction.
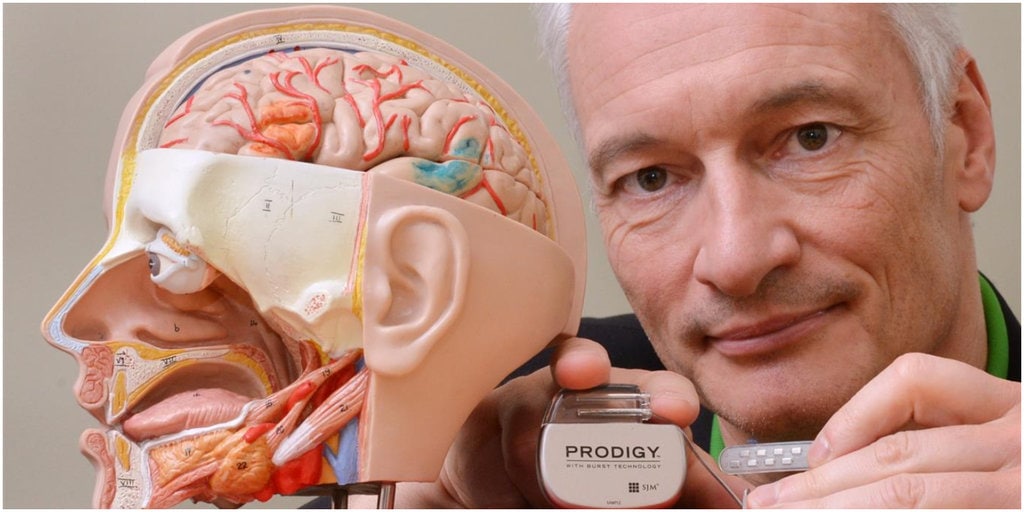
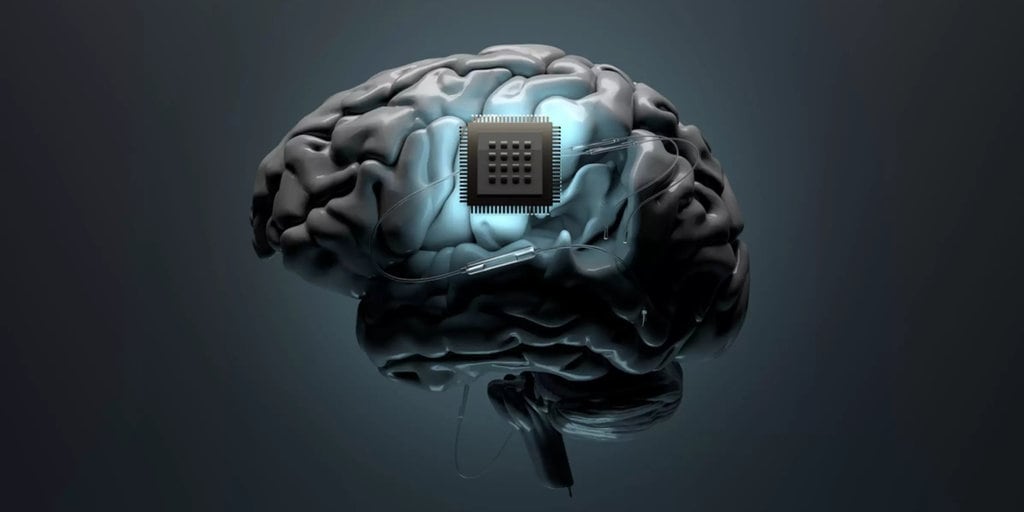
Brain implants, also known as deep brain stimulation (DBS) devices, have primarily been used to treat neurological disorders like Parkinson’s disease and epilepsy. However, scientists are now exploring their application in addiction therapy. These implants work by delivering electrical impulses to specific regions of the brain involved in addiction, modulating neural activity and potentially disrupting addictive behaviors.
One pioneering study featured in Smithsonian Magazine highlights the promising results of DBS in treating addiction. Researchers conducted trials on individuals with severe substance use disorders, targeting the nucleus accumbens, a brain region associated with reward and motivation. By stimulating this area with electrical pulses, participants experienced reduced cravings and improved control over their addictive behaviors, offering a glimmer of hope for those struggling with addiction.
Challenges and Considerations in Implementing Brain Implants for Addiction
While the potential of brain implants in addiction treatment is exciting, several challenges and ethical considerations must be addressed before widespread implementation. Firstly, the long-term effects and safety of DBS for addiction remain largely unknown. The brain is a highly complex organ, and altering its activity with electrical stimulation could have unforeseen consequences.
Additionally, the cost and accessibility of brain implant therapy pose significant barriers to its adoption. DBS procedures are invasive and require specialized medical expertise, making them inaccessible to many individuals, particularly those from marginalized communities. Moreover, the high cost of implantation and maintenance may limit its availability to those with financial means, exacerbating existing disparities in healthcare access.
Furthermore, ethical considerations surrounding consent and autonomy are paramount in the use of brain implants for addiction. Questions arise regarding the extent to which individuals can freely consent to undergoing invasive procedures, especially when grappling with the challenges of addiction. Ensuring that patients fully understand the risks and benefits of DBS treatment and providing adequate support throughout the decision-making process are essential ethical considerations. In conclusion, while brain implants hold promise as a novel approach to addiction therapy, significant scientific, ethical, and logistical challenges must be addressed before their widespread adoption. Collaborative efforts between scientists, healthcare professionals, policymakers, and ethicists are crucial in navigating these complexities and realizing the potential of brain implants in transforming addiction treatment.